In addition to onychomycosis, there are many other causes and diseases that can change the usual look of nails.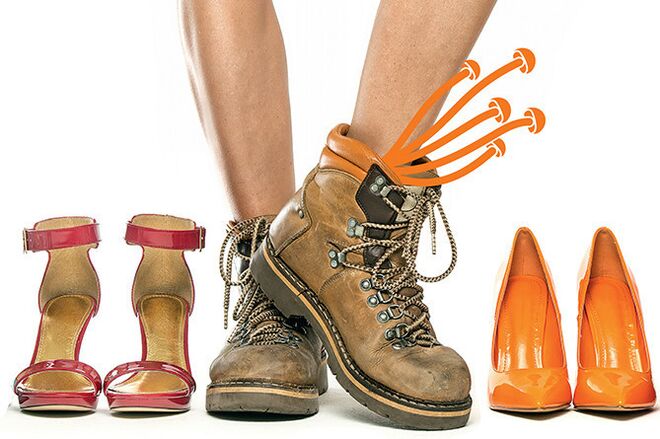 Thick, cloudy white nails can be the result of psoriasis or the unsuccessful use of harsh cosmetics. Detachment and delamination of the nail plate occur both with injuries and trophic diseases of the lower extremities with varicose veins or endocrine diseases. Onychomycosis very often begins not with changes in the nail plate itself, but with reddening, itching, and peeling of the skin surrounding the nail. If a person ignores these symptoms, the fungus begins to develop, invading deeper tissues, including under the nail bed. Fungal damage to the nail plate usually starts from its free edge, which thickens, turns grayish-yellow, easily breaks and crumbles. But even in this case, only with the help of laboratory research - microscopy - it is possible to accurately determine the presence of a fungus.
Thick, cloudy white nails can be the result of psoriasis or the unsuccessful use of harsh cosmetics. Detachment and delamination of the nail plate occur both with injuries and trophic diseases of the lower extremities with varicose veins or endocrine diseases. Onychomycosis very often begins not with changes in the nail plate itself, but with reddening, itching, and peeling of the skin surrounding the nail. If a person ignores these symptoms, the fungus begins to develop, invading deeper tissues, including under the nail bed. Fungal damage to the nail plate usually starts from its free edge, which thickens, turns grayish-yellow, easily breaks and crumbles. But even in this case, only with the help of laboratory research - microscopy - it is possible to accurately determine the presence of a fungus.
The fungus only occurs in the elderly and chronic patients.
In patients with chronic diseases (diabetes mellitus, peripheral vascular diseases, etc. ), nail fungus is really more common, but only for the reason that all these diseases reduce the activity of general and local immunity and affect the skin's resistance to infection. Age in itself may not be the cause of fungal diseases, but the older a person gets, the more health problems that contribute to the development of fungal infections accumulate. At the same time, completely healthy young people are not protected from onychomycosis. Sports enthusiasts can suffer from nail fungus. Calluses, microtraumas of the skin of the feet and sweating create ideal conditions for the development of fungi. The fungus can occur in people who spend most of the day on their feet, in closed shoes that do not allow excess moisture to evaporate. Smoking, frequent stress, and an excessive love of sweets increase the risk of developing fungal infections.
The fungus is usually contracted in a swimming pool, sauna, or beach.
In a sauna, a swimming pool or on the beach, the risk of encountering a fungus is really very high, as in any other place with high air temperature and humidity, where the spores of the onychomycosis pathogen remain viable for a long time. However, this is far from the only way you can get onychomycosis. The causative agent of fungal infections can get on the skin of a person who goes to a gym, beauty salon, shoe store, public transportation, or just wears someone else's slippers. However, contact with the fungus or its spores does not always lead to the development of an infection, much depends on the condition of the skin and the entire body. And only when the fungus enters the optimal environment for development and finds a weak point in the immune defense of the human body, it can damage the skin and nails. Risk factors for developing onychomycosis include dry calluses and cracks in the skin of the feet, increased sweating of the feet, wearing tight and "non-breathing" shoes and synthetic socks.
Fungal spores are everywhere, but there is no effective protection against them.
Fungal spores can actually be found almost everywhere, even at home, so contact with them cannot be completely ruled out. And yet a person at high risk of mycoses also has an opportunity to protect themselves from this infection. First of all, you need to carefully follow the rules of personal hygiene: use only your own shoes, towels, etc. It is equally important to carefully monitor the condition of the skin of the feet and nails - timely remove dry calluses, treat cracks and abrasions, andTo cut nails properly. There will be no redundancy in preventing excessive foot sweating, including using antiperspirant products for the feet. If the risk of onychomycosis is very high, you can prophylactically (once a week) cover your nails with a special antifungal varnish. You can also start taking drugs that increase immunity, after consulting your doctor - interferon inducers, drugs based on plant adaptogens, multivitamin complexes.
Mushroom is forever. You can't get rid of it entirely.
Onychomycosis is a common infectious disease that ends as soon as its pathogen is removed from the body. This can only be prevented by incorrect treatment or mistakes on the part of the patient himself. The peculiarity of onychomycosis is that the fungus is located under the nail plate (in the nail bed). Not every LP can penetrate that deep. Therefore, it is now recommended to use either special forms of external agents or systemic antifungal therapy to treat onychomycosis. In addition, treatment must continue even after all symptoms of the fungal infection have subsided. You can only stop taking medication if 3 repeated examinations (microscopy) show that the fungus is no longer in the tissue. In addition, the use of antifungal drugs must be combined with proper nail and foot care. this reduces the risk of new relapses.
There is no point in treating the fungus with external means.
Modern forms of external preparations make it possible to create a high concentration of an antifungal agent in the affected area. At the same time, external active ingredients are not absorbed into the systemic cycle, have a broader spectrum of activity and a lower risk of developing resistance. Unfortunately, not all external drugs can penetrate the thickness of the nail, especially the tissue of the nail bed, where the majority of pathogens are located. Therefore, it is recommended to combine local therapy with the removal of the nail plate or the use of keratolytic agents - urea or salicylic acid preparations. This is especially important when onychomycosis is accompanied by nail hyperkeratosis. Usually monotherapy with external agents is used in cases where the nails are affected by 1-2 fingers or 1/3 of the surface of the nail plates. In other cases, external agents are used in combination with systemic antifungal agents.
Antifungal pills are very dangerous and toxic.
Indeed, due to the long duration of antifungal therapy (in some cases up to 12 months), there is a risk of side effects and toxic effects on the liver. But today methods have been developed that will allow you to reduce this risk to a minimum. For example, some antifungal drugs are used in pulse therapy mode: d. H. short courses of 5-7-10 days with a break of 21 days. There are systemic antifungal drugs that can only be taken 1-2 times a week. There are antimycotics with a high safety profile which, in therapeutic doses, do not have any negative effects on the liver cells even after prolonged continuous use. Therefore, the most important thing is not to take systemic antifungal drugs without the appointment and supervision of a doctor. Only a dermatologist should prescribe such funds.
If you choose the right drug, the fungus can be cured in a week.
It is only possible to stop the development of a fungal infection in a short time if the infection has appeared recently and the causative agent of onychomycosis did not have time to penetrate deeply into the tissues surrounding the nail. Unfortunately, few patients seek medical help at this stage, most often treatment of onychomycosis begins in the later stages, when the nail plate (or even several) is severely affected and the process of dystrophy or hyperkeratosis is actively going on in the surrounding tissues. In such a situation, not a single drug will help quickly solve the problem of the fungus, even if the treatment is combined with the complete removal of the affected nail plate, because it takes about 3 months to restore the nail. In a relatively short time, around 4-6 weeks, you can reduce only the most noticeable symptoms of onychomycosis. However, the causative agent of the infection, especially in the form of spores, still remains in the tissue. And only after completing the treatment prescribed by the doctor can you get rid of this unpleasant disease.



























